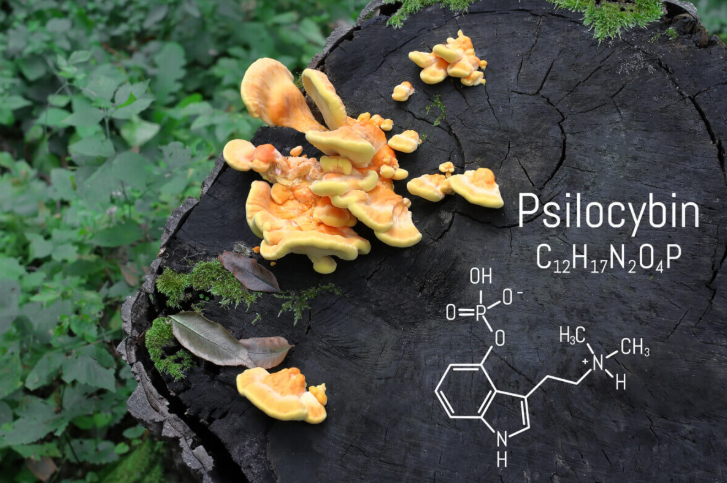
When patients with severe irritable bowel syndrome walk into Dr. Erin Mauney’s office, they’ve usually tried everything. Years of medications, diets, and treatments have failed them. So when she tells them she’s studying psilocybin — the psychoactive compound in magic mushrooms—to treat their gut problems, their reactions range from surprise to desperate hope.
Mauney, a pediatric gastroenterologist at Tufts University, is running the first study ever to test psychedelics on digestive disorders. Her research targets people whose irritable bowel syndrome (IBS) hasn’t responded to conventional medicine — a group that “may be 60%+ of patients by some studies,” according to Mauney.
The connection between psilocybin mushrooms and stomach problems might seem bizarre, but Mauney’s approach tackles something doctors have long overlooked: how psychological stress literally reshapes our gut function. Her patients often carry histories of childhood trauma that seem to manifest as physical symptoms decades later.
“I became very interested in the applicability of this emerging (or perhaps more apt to say, re-emerging) field of psychedelic-assisted medicine to patients who seem to be at war with their bodies,” Mauney explained in a recent interview published in the journal Psychedelics.
IBS causes unpredictable bouts of pain, cramping, diarrhea, and constipation that can derail careers and relationships. While the condition isn’t life-threatening, it can be socially isolating and emotionally devastating. Traditional treatments focus on managing symptoms rather than addressing root causes.
Mauney’s study examines something called interoception, which is how well people can sense and interpret signals from inside their bodies. Many IBS patients either become hyperaware of normal gut sensations, turning minor discomfort into severe pain, or completely disconnect from their bodily signals. Psilocybin appears to help reset this internal communication system.
Her research gives participants two doses of psilocybin alongside therapy sessions. Brain imaging using fMRI tracks changes in how patients perceive bodily sensations, while detailed interviews capture their reflections on the treatment.
Mauney’s path to psychedelic research began during the pandemic when she read Michael Pollan’s book “How to Change Your Mind.” As someone treating children and families dealing with mysterious symptoms, she started connecting childhood experiences to adult illness.
“During my medical training, I became aware of how common trauma, especially early life trauma, unfortunately is in the human experience,” she noted. “I think overall this is an area that medicine, particularly gastroenterology and obesity medicine, really fails to understand and address meaningfully.”
Her observation reflects growing scientific evidence that childhood experiences can affect adult health. Traditional medicine often treats physical symptoms separately from psychological causes.
While formal results haven’t yet been published, Mauney says sharing early observations with colleagues has been “very fun” — and appears to spark curiosity among other scientists. Rather than focusing solely on symptom relief, the study explores whether psychedelics can shift how patients relate to their bodily sensations in deeper, more meaningful ways.
Mauney draws from psychology literature, particularly the work of pediatrician-psychoanalyst Donald Winnicott, who explored how early relationships affect healing. Her interdisciplinary background allows her to see connections that purely medical approaches might miss.
Significant obstacles remain. Psilocybin is still federally illegal outside research contexts. Questions about optimal dosing, patient selection, and long-term effects need answers before treatments could become widely available.
But for patients who’ve exhausted conventional options, Mauney’s work offers hope. “This study brings a new option for patients who have not been helped by any existing approaches to IBS,” she said.
Rather than treating physical symptoms in isolation, Mauney’s approach recognizes that healing sometimes requires addressing the psychological experiences that may contribute to illness. For patients living with chronic digestive problems that conventional medicine struggles to solve, that holistic perspective could make all the difference.
Source : https://studyfinds.org/could-magic-mushrooms-help-ibs-psilocybin/











